
 Want to earn continuing education credit for this article? Learn more.
Want to earn continuing education credit for this article? Learn more.
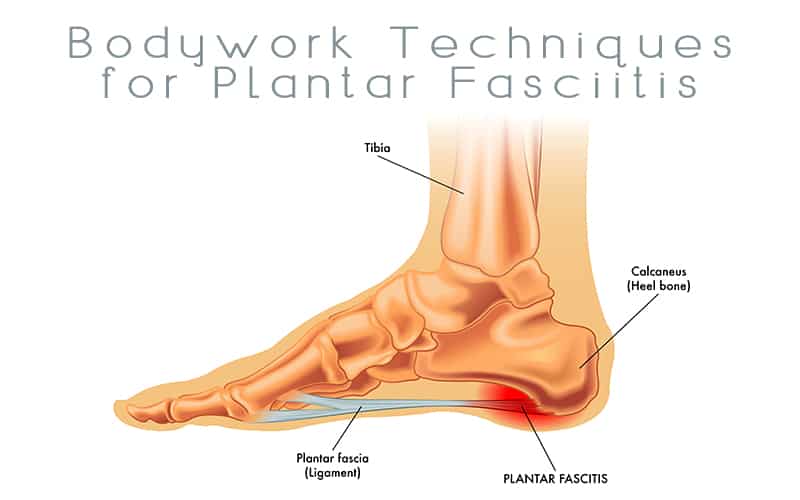
Plantar fasciitis is a common painful inflammation of the plantar fascia, the fibrous band of tissue on the sole of the foot. This tissue is instrumental in helping to support the arch and in acting as one of the body’s shock absorbers. Plantar fasciitis occurs when this band of tissue is overloaded or overstretched. This tension produces small tears in the fibers of the fascia, especially where the fascia meets the anterior calcaneous.
Plantar fasciitis is common in many types of people. Those afflicted include, but are not limited to, obese people, pregnant women, diabetics, people who repeatedly walk or stand on a hard surface, athletes and weekend warriors. In a pronated (low arch) foot, the fascia is under a constant stretch. In a supinated (high arch) foot, the fascia is under constant tension. Both of these arch extremes can easily lead to plantar fasciitis. Worn or poorly constructed shoes can contribute to the problem if they do not provide enough arch support, heel cushion or sole flexibility. In athletes, plantar fasciitis may follow intense training, especially in runners who push themselves too quickly to run longer distances.
The physiology of plantar fasciitis is a debated topic. It is widely acknowledged that this condition is associated with small tears in the fascia. However, further analysis of the tissue’s integrity is unclear. While the term uses the suffix -itis, indicating an inflammatory condition, many believe otherwise. Whitney Lowe, in issue #105 of Massage Magazine, says “There is mounting evidence that many common tendonitis complaints are actually not inflammatory problems at all, but instead are caused by a degeneration of the collagen matrix within the tissue. It has been suggested that plantar fasciitis is similar to these tendon pathologies, and that the problem is collagen degeneration in the fascial tissue.”
Symptoms of plantar fasciitis extend beyond foot pain following activity. According to Janet G. Travell, MD, and David G. Simons, MD, symptoms of plantar fasciitis primarily revolve around pain in the region of the plantar aponeurosis and/or pain in the heel. A unique characteristic of plantar fasciitis is marked pain upon arising in the morning. The first 10-12 steps are severely painful until the plantar fascia and the muscles have been stretched. The pain worsens again in the evening and after weight bearing activities.
Bodywork is extremely effective in helping people overcome the pain and limitations of plantar fasciitis. According to Art Riggs, Certified Advanced Rolfer, CMT, in his Deep Tissue Massage book, “The pain [of plantar fasciitis] is caused by tight and inflexible plantar fascia and, also by tight calf muscles. Medication and rest may improve symptoms, but if the causes are not addressed, the likelihood of recurrence is increased.”
In helping your clients overcome this condition, a focus on the plantar surface of the foot must be combined with lower posterior leg work. The posterior leg muscles attach via the achilles tendon to the calcaneous. Tightness in these muscles, mostly the gastrocnemius and the soleus, will pull on the calcaneous and add tension to the plantar fascia. It is recommended to have training in the individual bodywork techniques discussed below before applying them to your clients.
Plantar Surface of the Foot
- Glide on the plantar surface – Following some warm-up, glide your elbow, knuckles or thumbs from the foot pad to the heel. This will help the fascia migrate back up against the calcaneus. This can prevent heel spur development. Gliding on the lateral, medial and tranverse arches on the foot also contribute to relaxing of the plantar fascia.
- Mobilize the calcaneous – This method is courtesy of Riggs’ video series Deep Tissue Massage and Myofascial Release. With the client supine, cup your bottom hand between the ankle and heel. Use your upper hand to hold the distal part of the foot, including the ball of the foot and toes. Use your lower hand to create movement in the heel by rocking it side to side (medial and lateral) and even up and down (superior and inferior). Because the plantar fascia attaches to the calcaneous, this mobilization can aid in freeing up restrictions of the plantar fascia.
- Strip and stretch the plantar fascia – With the client supine, grasp the toes and ball of foot with one hand and dorsiflex the foot by stretching the plantar fascia. Use thumbs or knuckles to strip the plantar fascia from the ball of the foot to the heel. This may be very painful, but very helpful. Icing the foot afterward will speed the healing process.
- Deep transverse friction – According to Lowe, “Deep transverse friction may be used directly on the plantar fascia to stimulate fibroblast activity and tissue healing from chronic overuse. However, caution should be used in applying friction massage near the attachment on the calcaneous because of the possibility of a bone spur.” This technique can be very painful. Use the maximum amount of pressure tolerable to your client. Icing the foot afterward will speed the healing process.
- Wring the foot – The client is prone, with his/her knee at a 90-degree angle. Using a twisting motion, wring the foot as if you were wringing out a washcloth. This can be done for the entire foot, with one hand on the heel, and the other on the ball of the foot. This can also be done for the cuneiform joints, by having one hand on the ball of the foot, and the other on the center of the instep. As the muscles relax, you can increase the speed and intensity of the wringing to bring increased circulation and range of motion to the entire foot.
Posterior Lower Leg
- Myofascial release of the lower posterior fascial line – This technique is described in the Institute for Integrative Healthcare Studies’ Myofascial Release manual. Position your client prone with the foot off the table to assess the leg’s fascia. Cross your arms and place one hand on the calf (proximal to the belly of the gastrocnemius muscle) and the other on the lower leg (just proximal to the ankle). Stretch and wait for a release. Allow the fascia to unwind in its own time.
- Work the plantar flexors – With the client prone, put the Achilles tendon in a stretch by placing the client’s foot against your belly. Then use your thumbs to friction the sides of the Achilles tendon. Release the foot from your belly and use one thumb to push the tendon aside. Working at the level of the malleoli, rotate your other hand in order to cross fiber the anterior part of the Achilles tendon with your index finger. Follow with a forearm glide and/or stripping up the posterior leg being careful not to put pressure on the posterior knee.
- Treat trigger points – Use ischemic compression on trigger points of the soleus, gastrocnemius and flexor digitorum longus. James Mally, ND, in the Institute for Integrative Healthcare Studies’ Sports Massage manual, suggests having the client prone, pressing the trigger point, flexing the client’s knee and dorsiflexing the ankle. Then, Mally says to find the position where the client does not feel any pain in the trigger point (except if the point is in the soleus). Hold the point for 30-90 seconds or until a release is felt. Then bring the client back to a neutral position while continuing to hold the trigger point.
- Posterior fascial line stretch – Have your client stretch this line by performing a forward lunge, keeping the back leg straight and the feet flat on the floor. Hold for 20 seconds without any bouncing. Release for several seconds and repeat the stretch. This stretch can also be achieved by standing on the edge of a step. The balls of the feet are on the step while the heels hang off the step. Slowly, allow the body weight to shift into the heels, so that they drop below the step. This provides a great posterior lower leg stretch.
In addition to the above massage suggestions, here are some additional tips to offer your clients with plantar fasciitis:
- Rest is recommended for the acute stage.
- A physical therapist and/or athletic trainer can offer ultrasound, a stretching protocol, strengthening exercises and adequate taping.
- Supportive shoes or heel cups are helpful to many people.
- A podiatrist can fit your client for orthotics and/or a nighttime brace.
- Ice decreases inflammation and reduces the pain. Roll the foot over a firm cold object, such as frozen golf balls or a can of frozen juice concentrate.
- Surgery is available, hopefully as a last resort.
Plantar fasciitis is an increasingly common condition. An understanding of the anatomy and physiology of the foot and lower leg is very important in rendering appropriate care. Communication and collaboration with other healthcare professionals will provide your clients with the most comprehensive and effective treatment plan. Because massage therapists have such powerful tools to relieve plantar fasciitis, more bodyworkers will focus on and team up with professionals who treat this condition. Mastering the techniques described here, and making them your own, will give you a leg up on the pain of plantar fasciitis.
Earn continuing education credit for this article contained in our Foot Pathologies series. Click here to enroll.












Brilliant.